Antivenom is a specialized biological medicine made from purified antibodies that are designed to neutralize venom circulating in the human body. When a venomous animal bites or stings, toxins enter the bloodstream and begin attacking tissues, nerves, blood cells, or organs depending on the species involved. Antivenom works by binding to these toxins, preventing them from attaching to cells and causing further damage. Once neutralized, the venom–antibody complexes can be safely broken down and removed by the body.
For many venomous bites and stings, antivenom is the only definitive treatment. Supportive care such as pain relief, wound cleaning, and breathing assistance can help manage symptoms, but without antivenom, venom continues to spread and act on vital systems. Before the widespread availability of antivenom, mortality rates from certain snakebites were extremely high. In Australia, bites from species such as tiger snakes and taipans were often fatal, particularly in rural areas where medical care was delayed.
Modern medicine does not administer antivenom automatically after every bite. Doctors consider several factors before using it, including the species involved, the amount of venom injected, the patient’s symptoms, and how quickly those symptoms are progressing. Geography plays a critical role, as venom composition varies between species and even between populations of the same species in different regions. Administering the wrong antivenom can be ineffective or even dangerous, which is why careful assessment is essential.

Antivenom production relies on animals with strong immune systems capable of producing large quantities of antibodies. Horses are the primary animals used worldwide, particularly in Australia, due to their size, resilience, and ability to tolerate controlled exposure to venom over time. Their large blood volume allows for repeated plasma collection without harming the animal.
In addition to horses, other animals are sometimes used depending on the type of antivenom being produced. Sheep are commonly used for jellyfish antivenom, rabbits are used for funnel web spider antivenom, and dogs have been used in Australia for paralysis tick antivenom. The choice of animal depends on immune response, antibody quality, and safety considerations.
How is antivenom made?
The process of making antivenom begins with venom extraction. For snakes and funnel web spiders, venom is typically collected through a process known as “milking.” The animal is carefully restrained, and its fangs are encouraged to release venom into a sterile container. This procedure requires highly trained handlers, as the risk of envenomation is significant. Even experienced professionals face danger every time venom is collected.
For some animals, milking is not possible. Venom from creatures such as stonefish, redback spiders, and box jellyfish is obtained through dissection of venom glands after the animal has been humanely euthanized. These methods are carefully regulated and performed under strict laboratory conditions to ensure safety and consistency.
Once venom is collected, it is diluted and injected into the chosen animal in extremely small doses. These initial doses are far below levels that would cause harm. The animal’s immune system responds by producing antibodies specific to the venom’s toxins. Over time, the venom dose is gradually increased, allowing the immune system to strengthen its response without overwhelming the animal. This process can take months and requires constant veterinary supervision.
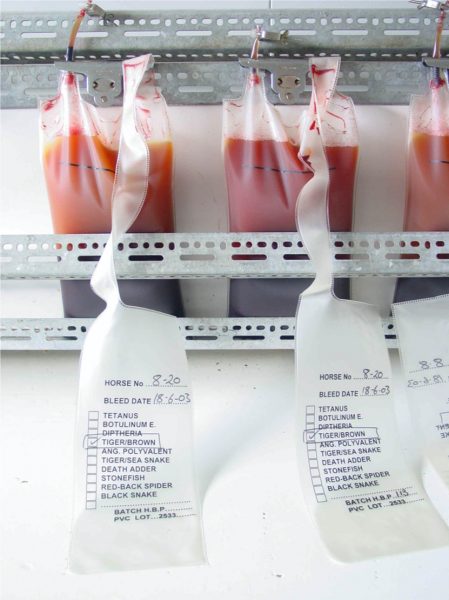
As antibody levels rise, blood is periodically drawn from the animal. The blood is then processed to separate plasma, which contains the antibodies. Red blood cells are typically returned to the animal to minimize stress and maintain health. The plasma undergoes further refinement, where unwanted proteins are removed and the antibodies are purified.
The purified antibodies may be modified to reduce the risk of allergic reactions in humans. This often involves fragmenting the antibodies into smaller, more targeted components that retain venom-neutralizing ability while being less likely to trigger immune responses. The final product is then sterilized, tested for potency and safety, and prepared for medical use.
Antivenom production is a slow, expensive, and highly specialized process, but it remains one of the most effective life-saving treatments in modern medicine. The quality and consistency of antivenom depend on rigorous scientific standards, careful animal care, and precise laboratory techniques.
Choice of antivenom and snake identification
Selecting the correct antivenom is one of the most critical decisions in treating a venomous snakebite. Different snake species produce venoms with distinct toxic effects, and antivenom is specifically designed to neutralize those toxins. Using the wrong antivenom may provide little benefit and can increase the risk of adverse reactions.
In some cases, the snake responsible for a bite is clearly identified. This may occur when the snake is captured, killed, or observed closely by someone experienced, such as a snake handler or wildlife professional. Under these circumstances, doctors can confidently choose the appropriate antivenom.
More often, however, identification is uncertain. Many bites occur at night, in dense vegetation, or when the snake is never seen at all. Even when a snake is observed, misidentification is common. Color patterns, size, and behavior can vary widely between species and even within the same species. Hospital staff and patients rarely have the training required to identify snakes accurately, and relying on guesswork can be dangerous.
For this reason, modern snakebite treatment focuses on clinical symptoms rather than appearance alone. Doctors assess signs such as paralysis, bleeding disorders, muscle damage, or neurological impairment to guide treatment decisions. In regions with multiple venomous species, this approach is often safer than visual identification.

Australia has developed a unique solution to assist with antivenom selection: the snake venom detection kit. This tool does not confirm whether venom has entered the body but helps determine which venom is present, allowing clinicians to select the most appropriate antivenom.
The detection kit works using a two-step enzyme immunoassay. Samples are collected from the bite site using a swab, and in some cases from blood or urine. These samples are then tested against antibodies that react specifically with venoms from different snake groups. A positive reaction indicates which venom family is involved.
It is important to note that the venom detection kit is not used to decide whether antivenom is needed. Instead, it is used to choose the correct antivenom once doctors have already determined that envenomation has occurred based on symptoms. Australia remains the only country in the world where such kits are routinely used in clinical practice.
Antivenom history and manufacturing background
The concept of antivenom dates back to the late nineteenth century. In the 1890s, researchers discovered that animals exposed to small, controlled amounts of venom developed immunity over time. One of the earliest pioneers in this field was Albert Calmette, who developed antivenom for cobra bites while working in what is now Vietnam.
Australia played a significant role in the early development of antivenom. In 1898, Frank Tidswell conducted pioneering experiments using tiger snake venom, laying the groundwork for modern antivenom production in the country. These early efforts dramatically reduced mortality rates from snakebite and established Australia as a leader in venom research.
Today, antivenom production in Australia is centralized under CSL Limited, which manufactures all Australian antivenoms. These products are widely regarded as some of the safest and most effective in the world, due to strict quality control, rigorous testing, and precise venom sourcing.
Australian antivenoms and production animals
Australian antivenoms are produced using different animals depending on the venom source. Horses are the primary animals used for most snake antivenoms due to their strong immune response and large blood volume. Other animals are selected based on how effectively they produce antibodies against specific venoms.
Snake antivenoms produced using horses include those for tiger snakes, brown snakes, taipans, black snakes, death adders, sea snakes, and polyvalent snake antivenom designed to neutralize multiple snake venoms.
Other Australian antivenoms include funnel web spider antivenom produced in rabbits, redback spider antivenom produced in horses, paralysis tick antivenom produced in dogs, box jellyfish antivenom produced in sheep, and stonefish antivenom produced in horses. Each combination reflects careful consideration of safety, immune response, and antibody effectiveness.

How to Make Antivenom
Antivenom technology
Modern antivenom production stands on more than a century of experimentation, trial, and refinement. One often-cited case that illustrates both the danger of venom and the power of antivenom is that of a man bitten by a cobra who survived due to rapid access to the correct treatment. Stories like this are not rare in regions where venomous animals are common, yet they highlight a much larger global problem: snakebite alone kills tens of thousands of people each year worldwide, with many more suffering permanent injury.
Despite its life-saving potential, antivenom remains scarce in many parts of the world. Production is expensive, technically demanding, and often unprofitable, which limits supply in regions where it is needed most. The basic idea behind antivenom, however, has changed little since the late nineteenth century, when scientists first realized that animals could be immunized against venom and their blood used to protect humans.
The earliest successful antivenoms were developed in the 1890s, when researchers demonstrated that antibodies produced in animals exposed to venom could neutralize toxins in bitten patients. While the tools and safety standards have evolved dramatically since then, the core biological principle remains the same. Modern laboratories now apply advanced purification techniques, strict quality controls, and detailed knowledge of venom chemistry to produce safer and more effective antivenoms than ever before.

Step 1: Milking the venom
The first step in antivenom production is obtaining venom from the target species. This process is commonly referred to as “milking,” and it is one of the most dangerous stages of antivenom manufacture. Venomous snakes are kept in controlled environments where their health is closely monitored, often undergoing quarantine and regular veterinary checks before venom extraction begins.
During milking, trained handlers restrain the snake and guide its fangs over a sterile collection container. Some facilities use protective equipment, while others rely on precise handling techniques developed over years of experience. In certain cases, mild electrical stimulation is used to encourage venom release, ensuring a consistent yield without harming the animal.
Milking techniques vary depending on the species. Rear-fanged snakes, for example, require specialized handling because their venom delivery system differs from that of front-fanged species. Coral snakes present another challenge, producing small quantities of highly potent venom. In some instances, thousands of milkings are required to produce enough venom for antivenom development, highlighting how resource-intensive this step can be.

Step 2: Cooling down and labeling
Once collected, venom must be stabilized immediately to preserve its biological activity. Fresh venom is typically cooled to very low temperatures, often around −20°C, to prevent degradation. In many cases, the venom is freeze-dried, a process that removes moisture while maintaining the structure of the toxins.
Freeze-dried venom is easier to store, transport, and measure accurately. Each batch is carefully labeled to record the species, subspecies, geographic origin, and date of collection. This information is critical because venom composition can vary significantly between populations of the same species living in different regions.
Proper storage and documentation ensure that antivenom produced later will be effective against the specific venoms responsible for bites in a given area.

Step 3: Choosing an animal for immunization
Selecting the right animal for antivenom production is a crucial decision. Horses are the most commonly used animals worldwide because they are large, resilient, and capable of producing high levels of antibodies. Their size allows for the collection of substantial volumes of plasma without compromising their health.
Other animals are used when horses are not ideal for a particular venom. Rabbits, sheep, and dogs have all been employed in antivenom production, depending on the immune response required and the intended use of the antivenom. Each species produces antibodies with slightly different characteristics, which can influence safety and effectiveness in humans.
There have even been experimental cases involving unconventional animals, but in practice, horses remain the backbone of global antivenom production due to their proven reliability and antibody yield.

Step 4: Immunizing
Immunization is the stage where the animal’s immune system is deliberately trained to recognize and respond to venom. Before injections begin, the venom is carefully prepared and diluted to levels that will stimulate antibody production without causing harm. In many cases, the venom is combined with adjuvants—substances that enhance the immune response and help the body produce stronger, longer-lasting antibodies.
Injections are administered in controlled doses and at specific sites on the animal’s body, often in the neck or shoulder area. The process follows a strict schedule, with doses gradually increased over time. This slow escalation allows the immune system to adapt safely, building a powerful defense against the venom’s toxins. Exact dosing schedules and preparation methods are closely guarded by manufacturers, as they directly affect antivenom quality.
Throughout immunization, animals are monitored continuously by veterinary staff. Blood tests are used to track antibody levels and ensure the animal remains healthy. It can take several months before antibody concentrations reach their peak. Once optimal levels are achieved, blood collection begins.
During collection, large volumes of blood may be drawn, but red blood cells are typically separated and returned to the animal to minimize stress and maintain long-term health. This process allows animals to continue contributing to antivenom production over many years.

Step 5: Purifying
After blood is collected, the plasma—rich in antibodies—is separated for purification. The goal of this stage is to isolate the antibodies that neutralize venom while removing proteins that could cause adverse reactions in humans.
The plasma undergoes a series of filtration and chemical processes to eliminate unnecessary proteins and contaminants. In many modern antivenoms, antibodies are enzymatically digested into smaller fragments. This step reduces the likelihood of allergic reactions and improves compatibility with the human immune system.
One widely known example of this approach is CroFab, a snake antivenom that uses enzyme-treated antibody fragments. Enzymes such as papain are used to cut antibodies into specific sections that retain venom-binding ability while reducing unwanted immune responses. These refinements have significantly improved the safety profile of antivenoms over older formulations.
Once purified, the antibody solution is sterilized and tested extensively. Quality control checks ensure potency, purity, and consistency from batch to batch. Only after passing strict regulatory standards is the antivenom approved for medical use.

Step 6: Human use
Once antivenom has been purified, tested, and approved, it is prepared for clinical use in humans. Antivenom is commonly supplied either as a liquid solution or in freeze-dried form. Freeze-dried antivenom has a longer shelf life and is easier to transport, especially to remote or rural areas where venomous bites are more likely to occur. Before administration, freeze-dried antivenom is reconstituted with sterile fluid under controlled conditions.
Antivenom is administered intravenously, allowing antibodies to enter the bloodstream quickly and begin binding to venom toxins. The timing of administration is critical. Antivenom is most effective when given as early as possible after envenomation, before toxins cause irreversible damage to organs, nerves, or blood cells. That said, antivenom can still be beneficial hours or even days later, depending on the venom involved and the patient’s condition.
Once in the bloodstream, antivenom antibodies circulate and attach to free venom molecules. This binding prevents venom from interacting with target tissues and allows the immune system to safely clear the venom–antibody complexes. Antivenom does not reverse damage that has already occurred, which is why early treatment significantly improves outcomes.
The number of vials required varies widely. Some bites may require only one or two vials, while severe envenomations can demand much larger quantities. In cases involving highly venomous snakes, such as certain rattlesnakes or taipans, treatment may involve repeated dosing based on symptom progression and laboratory results. Antivenom is expensive to produce, and individual vials can cost thousands of dollars, contributing to the high cost of treatment in some countries.
Despite its effectiveness, antivenom is not without risk. Because it is derived from animal antibodies, it can trigger allergic reactions in some patients. These reactions range from mild rashes and fever to severe anaphylaxis. Modern purification techniques have significantly reduced these risks, but patients are always closely monitored during and after administration. In hospital settings, emergency medications and equipment are kept on hand to manage adverse reactions if they occur.
Globally, access to antivenom remains uneven. In many regions where snakebites and other envenomations are most common, antivenom shortages persist due to high production costs, limited manufacturing facilities, and logistical challenges. This imbalance has led to preventable deaths and long-term disabilities, even though effective treatment exists.
There are also rare historical cases of individuals attempting to immunize themselves by repeated exposure to venom, with the idea of creating personal immunity. While such cases are often cited in popular stories, they are extremely dangerous and not medically supported. Antivenom used in hospitals is produced under controlled conditions, with precise dosing, purification, and testing that cannot be replicated safely outside a laboratory.
Antivenom remains one of the most remarkable examples of applied immunology in modern medicine. It represents a careful balance between biology, chemistry, animal care, and clinical practice, turning some of the deadliest natural toxins into survivable medical emergencies through science and precision.